We have for many years carried and prescribed two brands of therapeutic pet foods (also known generically as prescription or veterinary diets) at Brownsburg Animal Clinic—Hill’s Prescription Diet and Royal Canin’s “veterinary range.”
Our veterinarians also prescribe Purina Pro Plan, but until now, we’ve kept very few Purina products in stock at the clinic.
All three of these leading brands’ specially-formulated therapeutic diets contain high-quality ingredients, meet stringent manufacturing standards and are generally proven to be beneficial. We wouldn’t prescribe them if they weren’t trustworthy and effective.
But in recent months, we’ve seen such a sudden and substantial increase in Royal Canin’s prices that we’ve decided to switch over to Purina Pro Plan, along with Hill’s, as our two primary in-house brands, available for purchase at the clinic.
You can still buy all three brands’ regular and therapeutic formulas online for home delivery through our VetSource store.
All three companies’ products are available from other online retailers and area brick-and-mortar stores as well.
Why We Prescribe Therapeutic Diets
Even in a state of optimal health, what your pet eats has a direct impact on his or her vitality and wellbeing. For all pets, at all life stages, we recommend feeding good-quality, age-appropriate food from reputable manufacturers, and we’re happy to help you choose from among the many over-the-counter products.
To create therapeutic, prescription or veterinary diets, veterinary nutritionists manipulate nutrient levels and ingredients according to various tested formulas to benefit animals with a broad range of specific health conditions.
We prescribe therapeutic diets for pets we diagnose with conditions that have been shown to respond to these specially-formulated foods.
Specific conditions treated by therapeutic diets for dogs include:
- Anxiety
- Atopic dermatitis
- Cardiovascular disease
- Cognitive dysfunction syndrome
- Colitis
- Critical care
- Dental
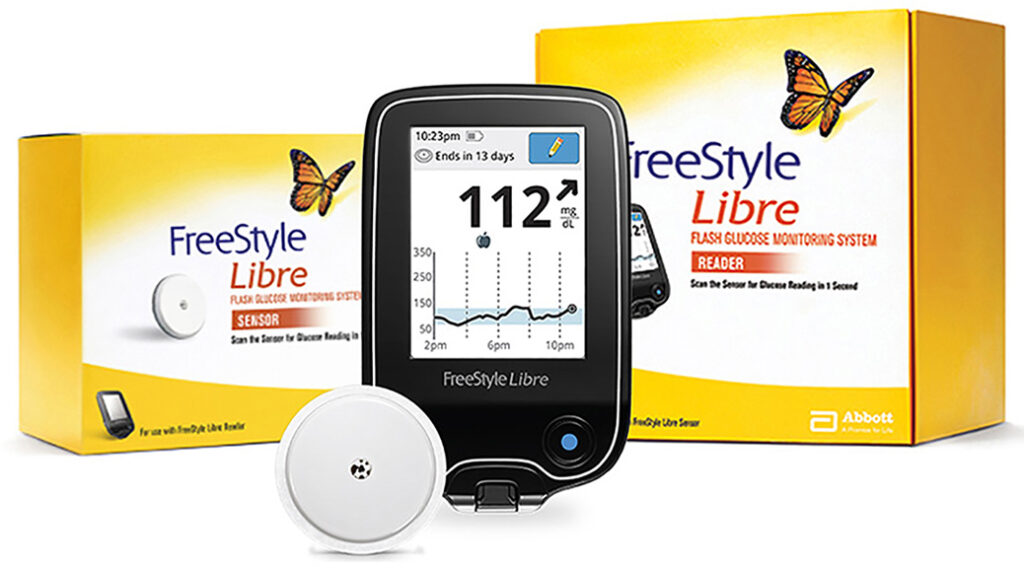
- Diabetes Mellitus
- Epilepsy
- Food allergy/food intolerance
- Gastrointestinal conditions
- Hepatic (liver) diseases
- Joint disease
- Obesity
- Oxalate stones (urolithiasis)
- Renal (kidney) disease
- Struvite stones (urolithiasis)
Conditions treated by therapeutic diets for cats:
- Constipation
- Critical care
- Dental
- Diabetes mellitus
- Food allergy/food intolerance
- Gastrointestinal conditions
- Hepatic (liver) diseases
- Obesity
- Oxalate stones (urolithiasis)
- Renal (kidney) disease
- Struvite stones (urolithiasis)
Hill’s Prescription Diet, Purina Pro Plan and Royal Canin offer products to provide tailored nutrition for pets with these conditions. If your veterinarian diagnoses any of these conditions and recommends a therapeutic diet, with a few exceptions, you’re likely to have a choice of at least two and more often three brands and, perhaps, multiple products within the brands to compare. Many formulas are available as both canned wet food and dry kibble.
What Therapeutic Diets Are Not
The Food and Drug Administration does not consider therapeutic diets to be “drugs” and does not legally require they be sold by prescription only. It’s the manufacturers and retailers who have chosen to require a prescription from a veterinarian before therapeutic foods can be sold.
Therapeutic diets are not medicine. They do not contain drugs or ingredients not also used in over-the-counter pet foods. They are more like nutraceuticals—digestible products similar to therapeutic vitamins and minerals that can support and influence your pet’s biological functions. The tested and demonstrated health benefits come from the precise combination of ingredients formulated by veterinary nutritionists to provide the best possible dietary support for pets diagnosed with the targeted medical conditions.
Therapeutic diets don’t cure diseases. They help us manage them. We use them as a complement to—not a substitute for—more comprehensive medical treatment.
As a rule, these deliberately formulated diets are not appropriate and may even be harmful for pets not diagnosed with the medical problem the diet is intended to support. Some are intended only for short-term use, while others may continue to benefit your pet indefinitely. Your veterinarian will monitor your pet and advise how long to continue with a therapeutic diet.
Marketing strategies aside, we believe this by-prescription-only policy helps minimize possible misuse of therapeutic diets by pet owners who might be tempted to feed them without first seeking sound medical advice and supervision. If your pet has a health issue that warrants a special diet, your veterinarian should be involved in definitively diagnosing the condition, recommending the right food and monitoring the diet’s impact on your pet over time.
Why Therapeutic Diets Cost More Than Regular Pet Food
As the ingredients lists show, therapeutic diets are made of essentially the same foods and nutrition supplements as regular pet foods.
It’s not the ingredients that make these foods cost more. It’s the science behind the formulation, quality control, testing and tweaking to produce the most medically beneficial results.
Before bringing a therapeutic diet to market, the manufacturer must show through extensive testing that it’s safe and effective for pets with specific conditions.
Contrary to fairly common belief, therapeutic diets are not big money-makers for most veterinary practices—ours included. Our mark-ups on these products are typically less than mark-ups on the regular pet foods you buy at the grocery or big box store.
We keep the most commonly-prescribed products in inventory for our clients’ convenience and to get our patients started on their prescription food without delay. In our online store, we aim to keep our prices in line with leading online retailers.
Our Advice to the Cost-Conscious
Given that specialized therapeutic diets tend to cost more than regular-formula pet foods, we understand feeding your pet a prescription diet—especially if needed over the long term—can strain your budget.
After the first bag or case of canned food is finished, you may even be tempted to switch back to regular food, saving you money but depriving your pet of the potential health benefits of the prescribed diet.
Like you, we want what’s best for your pet and your budget. That’s why, if you want or need to be especially price-conscious about your pet’s therapeutic diet, we encourage you to price-shop all three leading brands—Hill’s Prescription Diet, Purina Pro Plan and Royal Canin—and talk to your veterinarian about costs relative to quality and effectiveness of one brand’s equivalent or similar formula over another.
All else being equal, so long as the proposed product benefits your pet—our patient—we’re happy to consider prescribing the brand that helps you save some money.
Therapeutic Diet Price-Shopping Tips
There are hundreds of therapeutic pet foods on the market. If you’re shopping online, begin by using filters to display only foods meant for your pet’s specific health condition.
And yes, we know in your online shopping you will encounter more than the top three competing brands of dog food offering therapeutic formulas of their own. Once you’ve narrowed your choices by health condition, we recommend filtering out all but the three leading brands—Hill’s Prescription Diet, Purina Pro Plan and Royal Canin.
These are the brands our veterinarians know best and trust most. These are the brands we’ve prescribed for countless pets and can confidently recommend to you.
Base your price comparison on unit cost—the cost per pound or ounce—in all the available sizes. Click through as needed to see package size options for your pet’s prescribed food.
As a rule, larger sizes cost less per pound. If you’re looking only at the price-per-pound for the smallest sized packages, you’re likely seeing the highest unit prices.
Note, too, that each of the three manufacturers’ smallest available size is different. For one therapeutic dry dog food variety, for example, Purina Pro Plan’s smallest bag is 6 pounds at $7.67 per pound, while Royal Canin’s is 7.7 pounds at $6.10 and Hill’s is 8.5 pounds at $5.41.
In the largest available sizes, the per-pound prices drop from $7.67 to $3.69 for Purina, $5.41 to $4.18 for Hill’s and $6.10 to $4.32 for Royal Canin. Yes, Purina Pro Plan’s unit cost is highest among the smallest sized bags the three brands offer, but in the largest sizes, Purina has the lowest cost per pound.
So it pays to size-shop, too!
As you narrow your choices, the best way to learn about and compare individual products is by visiting the manufacturers’ websites.
To shop for Hill’s Prescription Diets for dogs, visit the dog products page with the “Prescription Diet” filter selected and check the “Health Category” option for your pet. Hill’s Prescription Diet products for cats are here. Shop for Hill’s products in our online VetSource store. On the Hill’s site, choose the “Buy Online” button to see other online retailers offering the product you need.
To shop for Purina Pro Plan therapeutic diets, visit the company’s products page for dog foods or cat foods, select the “Health Benefit” menu option in the left sidebar and choose your pet’s health condition. Purina’s “Buy Now” buttons take you to a map showing area retailers and online stores carrying the brand. Search “Purina Pro Plan” in our online store to shop there.
To shop for Royal Canin “precision veterinary dog diets,” visit the dog products page and select your pet’s “Specific Needs” in the left sidebar. Royal Canin’s precision veterinary cat diets products page shows the company’s full line of products for cats. The “Find a Retailer” button on individual product pages displays veterinary practices in your area that sell the food as well as area retailers. Royal Canin products are also available in our online store.
Changing From One Food to Another
Whether you’re changing from over-the-counter pet food to a therapeutic diet or switching between therapeutic diet brands, unless your veterinarian advises otherwise, make the transition slowly over a week or two.
Gradually decrease the old diet while increasing the proportion of the new until the transition is complete and you’re feeding the replacement food exclusively.
Make sure healthy pets in the household don’t have access to the therapeutic food. Feed it only to pets who have been diagnosed by a veterinarian who prescribed the diet specifically for that pet.
But Is It Tasty?
Some therapeutic diets don’t taste as good to pets as others. Cost considerations aside, your pet may prefer one brand’s flavor over another.
To derive the benefits of the prescribed food, your pet has to eat it, so before you commit to a $100+ bag of any particular prescribed diet, you may want to try the smallest size first to make sure your pet finds it tasty.
If your pet won’t eat the prescribed food, ask your veterinarian about possibly more palatable alternatives.
More Resources
For comprehensive brand comparisons, including discussion of regular as well as therapeutic formulas, check out these articles:
“Best Quality Dry Dog Food: Royal Canin vs. Hills Science Diet vs. Purina Pro Plan?”
“Science Diet vs. Purina Pro Plan: Who Wins? [2024]”
“Purina Pro Plan vs Hill’s Science Diet Dog Food: Our 2024 Comparison”
“Royal Canin vs Purina Pro Plan Dog Food: Our 2024 In-Depth Comparison”
“Purina Pro Plan vs. Royal Canin: Who Wins? [2024]”
“Science Diet vs. Royal Canin: Who Wins? [2024]”
You’ll find some repetition and contradictions among the articles, along with plenty of commission-earning affiliate links, but as you narrow your choice of products to discuss with your veterinarian, these exhaustive reviews can help you identify your own concerns and raise the questions most important to you at your next clinic visit.